Booster shot improves immune response of chemotherapy patients
A new study helps quantify the improved protection against COVID-19 achieved with a third booster dose of the vaccine from Pfizer Inc (PFE.N) and BioNTech SE in cancer patients who are undergoing chemotherapy. "Chemotherapy can weaken the
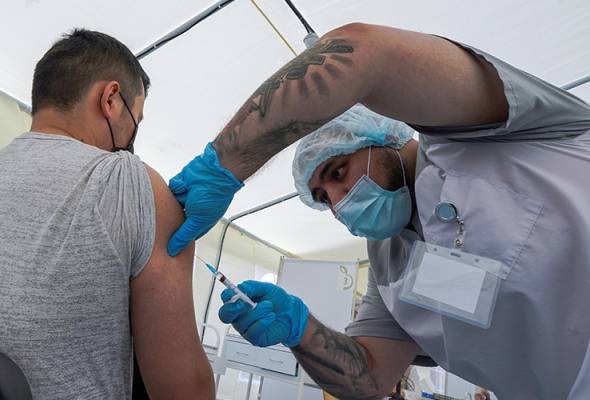
A new study helps quantify the improved protection against COVID-19 achieved with a third booster dose of the vaccine from Pfizer Inc (PFE.N) and BioNTech SE in cancer patients who are undergoing chemotherapy. “Chemotherapy can weaken the ability of cancer patients to fight off infections and to respond appropriately to vaccines,” said Deepta Bhattacharya of the University of Arizona College of Medicine, co-author of the study reported in Nature Medicine.
Her team studied 53 patients receiving chemotherapy for solid-tumor cancers who received two shots of the vaccine. Almost all of the subjects had an immune response after vaccination. But “the magnitude of these responses was worse than in people without cancer in almost every metric that we measured,” Bhattacharya said.
“In all likelihood, this leaves cancer patients more susceptible to infection and COVID-19 than healthy vaccinated people.” The researchers were able to bring back 20 of the study participants for a third vaccine dose, to see if immune responses would improve. “The levels of antibodies improved in about 80% of the cancer patients,” Bhattacharya said. “Our data on cancer patients supports the CDC’s broad guidelines that people who are immunocompromised should receive a third dose of the Pfizer vaccine.”
A small Italian study suggests that Lingering depression in COVID-19 survivors may be highly treatable. Doctors treated 58 patients who had developed post-COVID depression with a widely used class of antidepressant drugs known as selective serotonin reuptake Inhibitors, or SSRIs. These include sertraline, sold by Pfizer under the brand name Zoloft, GlaxoSmithKline’s (GSK.L) Paxil (paroxetine), Eli Lilly and Co’s (LLY.N) Prozac (fluoxetine) and Celexa (citalopram) from AbbVie’s (ABBV.N) Allergan unit. Usually, about 66% of patients see improvement with SSRIs, but among those with post-COVID-19 depression, 91% responded to treatment within four weeks, researchers reported this week at the European College of Neuropsychopharmacology meeting in Lisbon. They speculate that depression after COVID-19 is related to inflammation caused by the coronavirus, and note that SSRIs have some anti-inflammatory and antiviral properties. Dr. Livia De Picker of the University of Antwerp in Belgium, who was not involved in the study, said in a statement that the findings are particularly important for survivors with the syndrome of persistent symptoms known as Long COVID, which often includes depression.
Vaccinated individuals should continue to wear masks in public because they can still carry – and possibly shed – as much virus as unvaccinated people and not realize it, data from a new study confirms. Researchers studied viral levels at diagnosis in 869 patients, including 632 who were asymptomatic. Most of the infections were caused by the highly contagious Delta variant of the coronavirus. They found no statistically significant differences in average viral loads between vaccinated and unvaccinated individuals, or between those with or without symptoms, or among different age groups, genders, or vaccine types. “Our study does not provide information on infectiousness,” said Richard Michelmore of the University of California, Davis, noting that virus transmission is influenced by several factors, not just vaccination status and viral load. “It is not OK to assume that because you are vaccinated that you cannot become infected and cannot infect someone else, even if asymptomatic,” he said. COVID-19 vaccines do decrease the odds of infection and reduce infection severity. However, people vaccinated against COVID-19 should still wear masks in public because they might infect others if they themselves become infected, researchers advised.






