CMRI Introduces Endoscopic Bariatric Surgery: Shed Pounds with No Scars. Only Laughs!
Dr. Sarfaraz Baig, Senior Consultant - GI Surgeon, Department: Bariatric and Hernia/ AWR Surgery In the 'Obesity' pandemic, Dr. Baig suggests a collaborative effort from public and private sectors is crucial. While prevention is key, treating
Dr. Sarfaraz Baig, Senior Consultant – GI Surgeon, Department: Bariatric and Hernia/ AWR Surgery
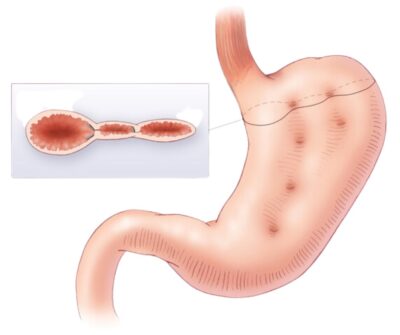
In the ‘Obesity’ pandemic, Dr. Baig suggests a collaborative effort from public and private sectors is crucial. While prevention is key, treating class 2 or 3 obesity often challenges traditional methods with a success rate of 1 in 100, and Laparoscopic Bariatric Surgery isn’t universally suitable due to surgical concerns. A promising alternative is Endoscopic Bariatric Surgery or Endoscopic Sleeve Gastroplasty, a non-surgical procedure using advanced endoscopy tools. It makes the stomach smaller, modifies eating capacity and gut signals, offering a viable option for those averse to surgery or needing modest weight loss in the battle against obesity.
Performing Endoscopic Bariatric Surgery involves inserting a slightly larger endoscope into the stomach with two channels. Utilizing advanced instruments, a needle holder with a stitch and forceps are employed for internal stomach stitching, offering a minimally invasive procedure akin to open or laparoscopic surgeries. Patients can go home the same day, devoid of abdominal scars, as the process occurs through the mouth. Recovery is swift with minimal pain, and though some may experience nausea and abdominal cramping for the initial 3-4 days, it subsides. Several clinical trials suggest significant weight loss with safety comparable to or even surpassing Laparoscopic Bariatric Surgery.
The strides in weight loss interventions owe their success to years of research, overcoming initial trials and skepticism. Over the past few years, numerous surgeries, including pivotal trials like the Merit trial, have contributed to establishing a commendable safety profile for the procedure. While diet and lifestyle modifications, coupled with physical training, form integral components of all treatment protocols, additional measures become imperative due to their limited effectiveness in isolation. For individuals in Class 1 obesity, the incorporation of anti-obesity drugs is considered, recognizing the availability of various medications. However, the potential side effects, costs, and issues of noncompliance associated with drugs make alternative interventions necessary. Endoscopic Bariatric Surgery emerges as a preferred non-surgical approach for class 2 obesity patients, offering rapid recovery and minimal discomfort. For those in Class 3 obesity, Laparoscopic Bariatric Surgery remains the favoured option for achieving significant weight loss.
All decisions regarding treatment options will involve mutual counselling and discussion with the patient. A Class 1 patient, for instance, whose diabetes drugs may not be effective, might choose Laparoscopic Bariatric over Endoscopic Bariatric. On the other hand, individuals in Class 3 or 4 obesity may opt for Endoscopic Bariatric if they are averse to surgical procedures. CMRI is among the first centres in India to adopt Endoscopic Bariatric Surgery, equipped with the necessary logistics and infrastructure. This approach is considered highly beneficial for society, especially for patients unwilling to undergo surgery. Dr. Baig highlights that, “On Monday, the 9th of January, we successfully conducted two cases under mentorship. The procedures went smoothly, and the patients were discharged the following morning without any complications, experiencing minimal pain.” The CMRI’s Specialist states that the first patient, a 35-year-old woman with a BMI of 39, struggled with obesity and infertility, and the second case involved a 29-year-old male.
Endoscopic Bariatric is an exciting breakthrough in weight loss interventions. This procedure is performed through an endoscope inserted down the mouth to the stomach, reduces the capacity to eat by stitching the stomach under anaesthesia. It’s a daycare procedure with low pain scores, quick recovery, and no scars. Ideal candidates are those with Class 1-2 obesity (BMI 30-40), with young
individuals showing particular interest. It proves effective for modest weight loss and is beneficial for conditions like uncontrolled diabetes, sleep apnea, and even for those facing infertility due to PCOD.